Cultural competency training is essential for healthcare providers to deliver effective therapy for adolescent teens psychosis, bridging cultural gaps in care and improving patient-provider relationships. By addressing biases, learning tailored communication strategies, and implementing stress reduction methods, providers can create safer spaces for vulnerable teens from diverse backgrounds. Comprehensive training programs, ongoing workshops, and measurement of effectiveness ensure professionals remain competent, empowering them to offer more accurate diagnoses and tailored therapies that address unique cultural expressions of distress.
Cultural competency in healthcare is essential, especially when addressing the unique needs of adolescent teens with psychosis. This article explores strategies to enhance cultural responsiveness among healthcare providers, aiming to improve diagnosis and treatment outcomes. We delve into the impact of biases, present training methods, and discuss evaluating program success. By understanding the intricacies of diverse cultures and their influence on mental health, therapists can provide tailored therapy for adolescent teens with psychosis, ensuring better access to quality care.
- Understanding Cultural Competency in Healthcare for Adolescent Teens with Psychosis
- The Impact of Cultural Biases on Diagnosis and Treatment
- Strategies for Training Healthcare Providers to Be More Culturally Responsive
- Measuring Effectiveness: Evaluating the Success of Cultural Competency Programs
Understanding Cultural Competency in Healthcare for Adolescent Teens with Psychosis

Cultural competency is an essential aspect of healthcare, especially when treating adolescent teens with psychosis. This involves understanding and respecting diverse cultural backgrounds, beliefs, and values to provide effective therapy for adolescent teens psychosis. Healthcare providers play a crucial role in bridging the gap between patients from different communities and delivering quality care. By incorporating cultural competency training, they can enhance their ability to communicate effectively using tailored communication strategies.
This training equips them with valuable tools such as conflict resolution techniques, enabling them to navigate sensitive situations and create a safe space for vulnerable teens. It’s not just about treating symptoms but also addressing the unique needs and challenges that arise from cultural differences in mental health care. Through this approach, healthcare providers can ensure more inclusive and accessible therapy for adolescent teens with psychosis, fostering better outcomes and improved relationships between patients and caregivers.
The Impact of Cultural Biases on Diagnosis and Treatment

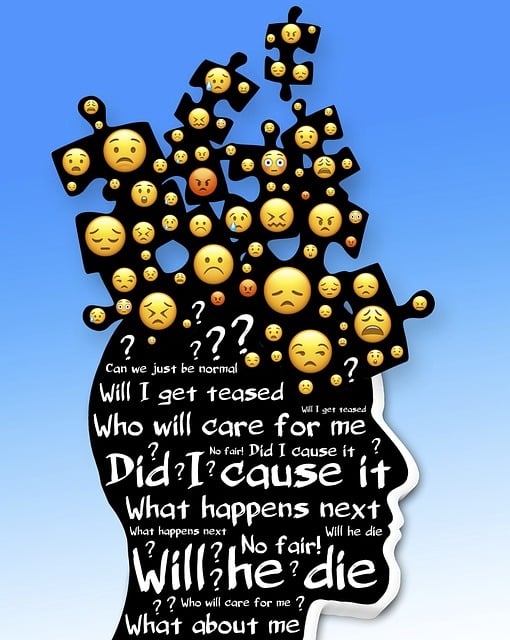
Cultural biases ingrained in healthcare systems can significantly impact diagnosis and treatment plans, particularly for adolescents experiencing psychosis. These biases, often stemming from stereotypes and generalizations about racial, ethnic, or cultural groups, can lead to misdiagnoses or delayed treatment. For instance, symptoms of psychosis in teens from minority backgrounds might be attributed to other causes due to societal misconceptions, resulting in a lack of appropriate mental health care. This phenomenon is not only a matter of equity but also a critical aspect of healthcare provider training, especially with the increasing diversity of patient populations.
Mental Health Policy Analysis and Advocacy plays a pivotal role in addressing these disparities by promoting inclusive practices. Training healthcare providers on communication strategies that bridge cultural gaps can enhance patient-provider relationships. By learning effective Stress Reduction Methods, professionals can create safer spaces for adolescents to openly discuss their experiences, which is essential when dealing with sensitive topics related to psychosis. Thus, competent cultural awareness fosters more accurate diagnoses and tailored therapies, such as those designed for adolescent teens experiencing psychosis.
Strategies for Training Healthcare Providers to Be More Culturally Responsive

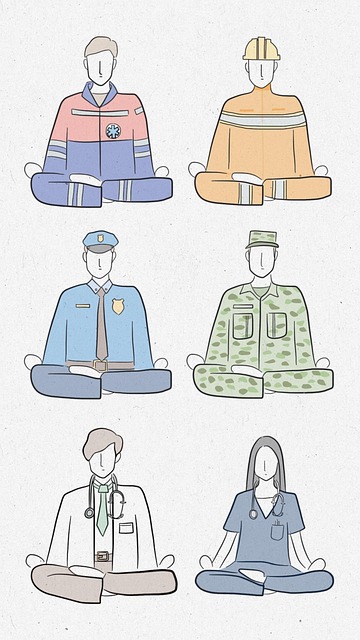
Training healthcare providers to be culturally responsive is a multifaceted approach that involves education, exposure, and empowerment. A robust healthcare provider cultural competency training program should incorporate diverse role-playing scenarios, where trainees practice navigating complex interpersonal dynamics with patients from various backgrounds, including those experiencing psychosis in adolescent teens. This hands-on method allows them to develop strategies for providing anxiety relief while respecting cultural beliefs and practices that may differ from their own.
Incorporating cultural sensitivity in mental healthcare practice means teaching providers about the impact of systemic biases and how they can unconsciously influence patient interactions. By fostering a deeper understanding of diverse communities, including their unique expressions of distress, providers can offer more tailored and effective therapy for adolescent teens experiencing psychosis. Ongoing workshops, mentorship programs, and continuous learning opportunities are essential to sustain cultural competency and ensure providers remain responsive to the evolving needs of their diverse patient populations.
Measuring Effectiveness: Evaluating the Success of Cultural Competency Programs

Measuring the effectiveness of cultural competency training is a critical step in ensuring its success and long-term impact on healthcare delivery. Evaluating these programs involves assessing both the knowledge gain among participants and their subsequent behavior changes when interacting with diverse patient populations. One effective method is through post-training assessments, where individuals are tested on their understanding of cultural nuances, biases, and strategies to improve care. These tests can include scenarios related to therapy for adolescent teens experiencing psychosis, a specific area that requires sensitive cultural approaches.
Additionally, tracking the implementation of skills learned in real-world settings is essential. This can be achieved through observation, feedback from patients and colleagues, and documentation of improved risk management planning as part of emotional regulation strategies. By incorporating these evaluation techniques, mental health professionals can enhance their practice, better serve diverse communities, and contribute to overall positive mental health outcomes.
Cultural competency training is a vital tool in enhancing healthcare delivery for adolescent teens with psychosis. By understanding and addressing cultural biases, healthcare providers can ensure more accurate diagnoses and tailored treatments. The strategies outlined in this article provide a framework for creating inclusive environments, fostering empathy, and improving patient outcomes. Measuring the effectiveness of these programs is crucial to identify areas of improvement, ensuring that training meets its goal of offering quality therapy for adolescent teens with psychosis and promoting culturally responsive care.